What is PTSD?
Post traumatic Stress disorder (PTSD) is a mental health diagnosis that can arise after an individual is exposed to a traumatic or life-threatening incident. Common events include sexual or physical assault, experiences in war, automobile accidents, natural disasters, etc.
The symptoms of PTSD can vary widely and may include disturbing thoughts, feelings and/or dreams and mental and/or physical distress. Not everyone who experiences a life-threatening incident will develop PTSD, but those who do tend to have a heightened and sometimes life- interfering desire to avoid similar situations in the future.
During World Wars I and II, returning veterans experiencing these symptoms were often referred to as experiencing “shell shock” or “combat neurosis”. The term Posttraumatic Stress Disorder was introduced after the Vietnam War, and was incorporated into the American Psychiatric Association’s’ Diagnostic and Statistical Manual in 1980.
To be Diagnosed with PTSD, an Individual Must Experience the Following for More Than a One Month Period:
One or more re-experiencing symptom. These can come sporadically and without warning and may induce panic attacks or other physical symptoms:
- Flashbacks where the individual re-experiences the trauma in waking life
- Bad dreams related to the incident
- Disturbing thoughts related to the event
One or more avoidance symptoms. These are often based on a specific incident and may greatly alter one’s day-to-day routine:
- Avoiding people, places, or things that remind them of the incident
- A feeling of numbness
- Feelings of worry, fear, or guilt
- Loss of passion for previously enjoyed life activities
- Any sort of “black out” or “blocking” of the memory of the event.
An example might be someone traumatized by a war zone avoiding a bowling alley for the loud sound of the pins falling, potentially reminding them of the sounds of war.
Two or more arousal/reactivity symptoms. These are often constant and may interfere with daily life:
- Startling easily
- Insomnia
- Emotional outbursts
- Feeling tense or being on edge
- Difficulty concentrating
Two or more cognition/mood symptoms. These may be constant and difficult for others to understand:
- Loss of enjoyment of activities
- Feelings of guilt
- Loss of memory about the event
- Depressed thoughts about themselves
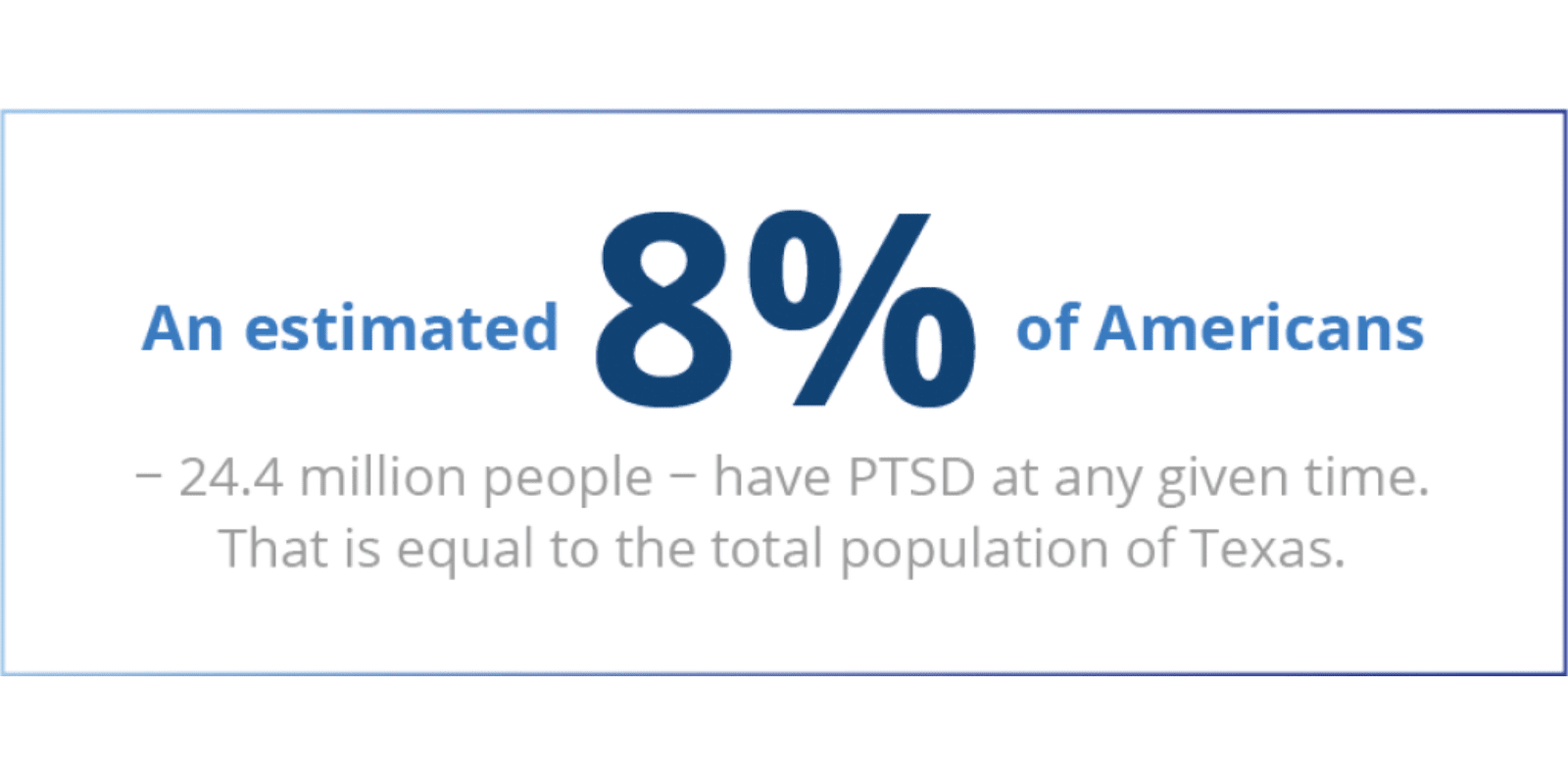
Who Does PTSD Affect?
Contrary to popular belief, Posttraumatic stress disorder is fairly common in the U.S. Women, people who have prior trauma history, people who have other mental health issues or use substances, and individuals with a fragile support network are often more likely to develop the disorder following a traumatic event.
While they would not technically fit current diagnostic criteria for the disorder, many children in America also struggle with PTSD-like symptoms as a result of various childhood traumas, including neglect, abuse, a dysfunctional family system, and more. In the brain, trauma can increase levels of the stress hormone cortisol as well as activity in the amygdala, (the fight or flight area of the brain).
These changes and their after-effects can carry over into the teen and young adult years, affecting an individual’s emotional, mental, and sometimes even physical development. In teens and young adults, the reaction to trauma can present as an increase in irritability in lieu of other emotional symptoms.
They may also experience something called post traumatic reenactment, or the compulsion to re-enact the trauma. An example of this would be a teen who was traumatized by a gunfight beginning to carry a gun.
PTSD and Substance Use
Given their symptoms, it is unsurprising that those experiencing PTSD often have an urge to reach for substances to cope. Depressants and other drugs that relax or soothe the nervous system in the short term are often employed to help an individual manage situations that may be triggering.
Stimulants or dissociatives may be used to combat depressive thoughts. As with most co-occurring disorders, this can lead to larger issues down the road:
Bypass true healing
The individual may bypass the opportunity to truly heal the PTSD (for which there are a number of effective therapies) by minimizing the symptoms.
Increase negative symptoms
The use of substances may increase negative PTSD symptoms; in the short term a substance may provide relief but as the body/brain learns to lean on the substance, the stress to obtain it may increase and coping skills other than substance use decrease.
Brain rewiring
As with most substance use, the brain may be re-wired for reward-based circuitry. This can decrease an individual’s ability to delay gratification or manage short term stress.

PTSD & Drug Addiction Treatment
As with other anxiety disorders, PTSD can be seen as our bodies’ natural, intelligent attempt to protect us from harm. If you or a loved one has experienced a traumatic event and/or is exhibiting the symptoms above, or been diagnosed with PTSD, know that care is available.
While individuals sometimes turn to substances to “self-medicate,” or manage their symptoms, this often only makes matters worse. The sooner you seek PTSD care, the more you or your loved one is set up for a long-term and sustainable recovery.
Our team is dedicated to serving individuals and families with substance abuse and the challenges of co-occurring disorders.

Online Treatment Programs
Our virtual IOP program offers the same programming that we offer in person, all online – this is ideal for those who live too far to drive to an addiction center, have transportation issues, or have health concerns that make in-person treatment challenging.
Our Accreditations