The Main Types of Depression According to the DSM-5
When people think of depression, what often comes to mind is what is known as major depressive disorder (MDD).
MDD is a form of depression characterized by symptoms such as a low mood that lasts for several weeks. Along with emotional symptoms, you can also experience physical symptoms like an increase or decrease in appetite.
However, the Diagnostic and Statistical Manual of Mental Illnesses, or DSM-5, recognizes several different types of depression.
Depressive disorders in the DSM-5 include:
- Major Depressive Disorder
- Persistent Depressive Disorder (Dysthymia)
- Disruptive Mood Dysregulation Disorder
- Single and Recurrent Episodes
- Premenstrual Dysphoric Disorder
- Substance/Medication-Induced Depressive Disorder
- Depressive Disorder Due to Another Medical Condition
- Other Specified Depressive Disorder
- Unspecified Depressive Disorder
Note: Sometimes individuals with depression experience thoughts of death, dying, and suicide. If you or someone you care about is experiencing suicidal thoughts, seek emergency medical treatment by calling 911 or going to an emergency department.
Major Depressive Disorder
Major depressive disorder (MDD), also referred to as major depression, unipolar depression, or clinical depression, is one of the most common types of depression.
It is a common mood disorder. Each year, approximately 15.5% of adults in the United States experience MDD, and it is also one of the leading medical causes of disability.
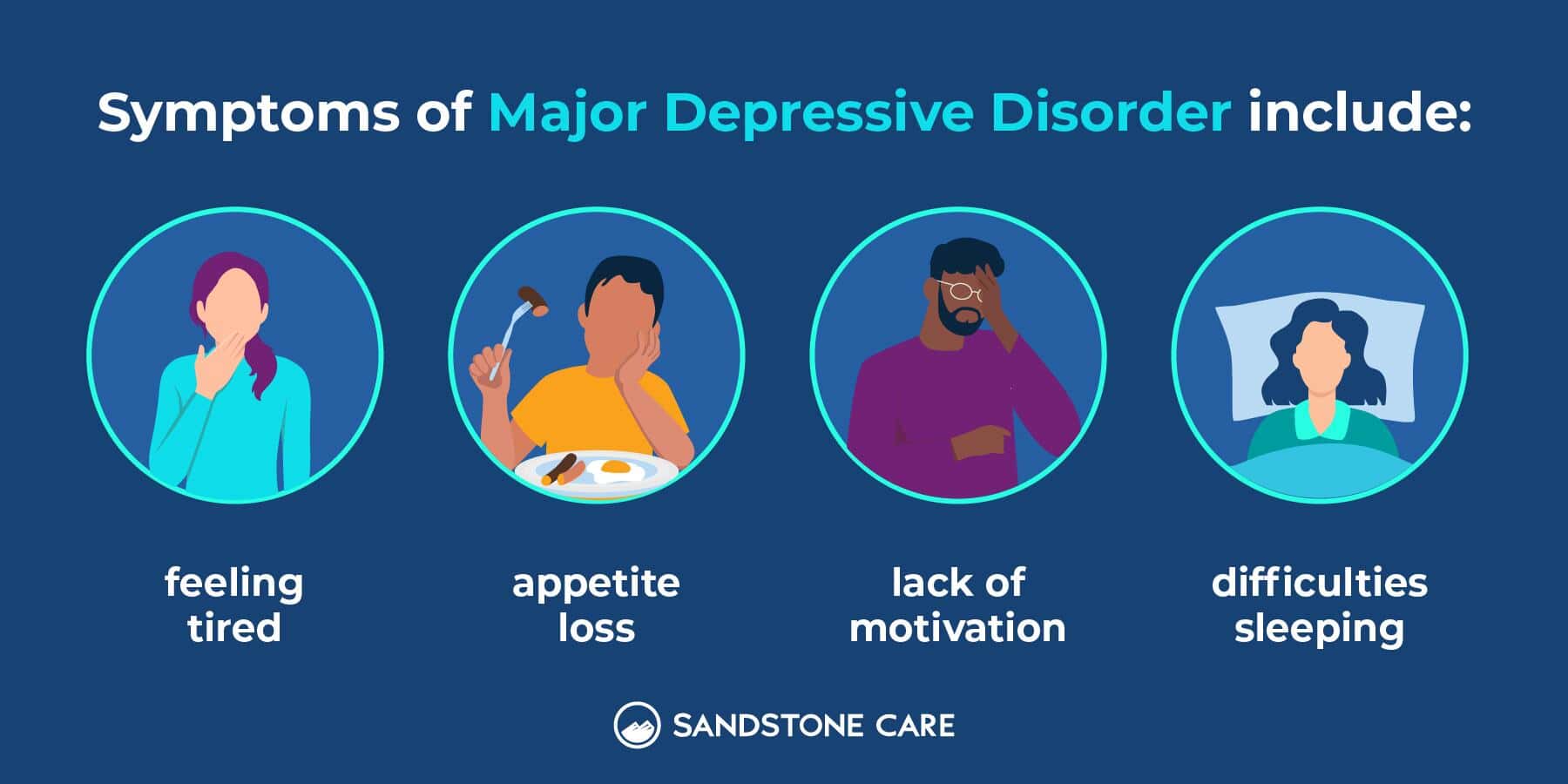
Symptoms of MDD include:
- Feeling tired
- Weight loss
- Appetite loss
- Loss of pleasure from activities
- Lack of motivation
- Difficulties sleeping
- Cognitive issues (e.g., difficulty concentrating)
- Emotional challenges (e.g., feeling guilty over minor issues)
- Low mood
Treatment of MDD depends on the severity of the depression. Treatment often includes antidepressant medication, psychotherapy such as talk therapy or cognitive behavioral therapy (CBT), or a combination of the two.
In MDD, the depressive episodes last at least two weeks, and the symptoms affect multiple areas of daily life.
While many will recover from the initial episode, recurrent episodes are common. Up to 40% of individuals will experience another depressive episode within two years.
Chronic Depression: Persistent Depressive Disorder (PDD)
Persistent depressive disorder (PDD) is a chronic, ongoing form of depression.
PDD used to be called dysthymia. Dysthymia is a Greek word meaning “despondent” (hopeless or low state).
A family history of PMDD and being female are risk factors. PMDD is more common in females than in males and the condition can last for years.
While some people respond well to treatment, this condition is more challenging to treat, and symptoms may persist.
Symptoms of PDD: The main symptom of PDD that differentiates it from other forms of depression is a low or depressed mood on most days lasting at least two years.
In kids and teens, it’s essential to understand that depression can present as irritability rather than a low mood. Also, in kids and teens, a provider can diagnose PDD after one year of symptoms, instead of two.
Other symptoms, which are similar to those of MDD, include:
- Difficulties with sleep (sleeping too little or too much)
- Feeling hopeless
- Eating too little or too much
- Low energy
- Difficulty concentrating or focusing
Treatment of PDD includes lifestyle changes, medication, and psychotherapy.
Medications are not always as effective for PDD as they are for MDD and may take longer to work. It is important to continue taking your medications as prescribed and talk to your healthcare provider if you have concerns about their effectiveness.
Disruptive Mood Dysregulation Disorder (DMDD)
Disruptive mood dysregulation disorder (DMDD) is a depressive disorder diagnosed in children between the ages of 6 and 10 years.
It is a newer disorder, recognized in the DSM-5 for the first time in 2013.
Symptoms: While outbursts and tantrums are normal in kids, DMDD is a condition where kids have outbursts that are out of proportion to what happened.
This can look like:
- Frequency: Severe temper tantrums or outbursts three or more times per week. The outbursts can be verbal, physical, or a combination of the two.
- Duration: The outbursts and tantrums have occurred for at least 12 months
- Mood: Irritable or angry mood most days for the majority of the day
- Difficulty functioning: Challenges in more than one area (e.g., school and home) due to the irritable mood
Treatment: Since DMDD is a condition that affects children, parents and caregivers play an essential role.
Treatment may include:
- Psychotherapy: CBT may help kids build tolerance for frustration without having an outburst.
- Medication: As of 2025, there are no Food and Drug Administration (FDA) approved medications to treat DMDD. However, medicines that are used and may be helpful include stimulants, antidepressants, and atypical antipsychotic medications.
- Parent and caregiver coaching: How parents and caregivers respond to outbursts can influence the condition. Teaching parents and caregivers more effective strategies when outbursts do occur, as well as ways to reduce them in the first place, is considered an important part of treatment.
It is essential to work closely with the child’s healthcare provider. As children grow up into adolescents and teens, the frequency of tantrums may decrease. However, children with DMDD are at a greater risk of developing anxiety and depression.
Premenstrual Dysphoric Disorder (PMDD)
Premenstrual Dysphoric Disorder (PMDD) is a cyclical condition that is similar to premenstrual syndrome (PMS), but with more severe symptoms.
Hormonal fluctuations, as well as fluctuations in serotonin that occur during a female’s menstrual cycle play a role in the development of PMDD. Females with PMDD may be more sensitive to these changes.
The condition is diagnosed when five or more symptoms are present, with at least one mood-related symptom.
Symptoms can include:
- Irritability and anger
- Panic attacks
- Difficulty focusing
- Anxiety
- Feeling sad
- Difficulty sleeping
- Food cravings, increased appetite, or binge eating
- Severe mood swings
- Crying
- A sense of being out of control
- Trouble sleeping
- Loss of interest in daily activities
- Typical period symptoms such as cramps, breast tenderness, and bloating
Treatment often includes a combination of therapies, such as:
- Medications: Antidepressants, especially selective serotonin reuptake inhibitors (SSRIs), are often used to treat PMDD.
- Birth control pills: A specific birth control pill containing the hormones drospirenone and ethinyl estradiol is used for PMDD treatment.
- Over-the-counter (OTC) medications: OTC medications such as acetaminophen (e.g., Tylenol) and ibuprofen (e.g., Advil) can help to relieve physical period symptoms such as cramps and headaches.
- Lifestyle interventions: Making healthier food choices (e.g., cutting back on fried or sugary foods), focusing on quality sleep, engaging in exercise, and stress management activities such as deep breathing may also help.
Other DSM-V Depressive Disorders
The other depressive disorders included in the DSM-5 are:
Substance/Medication-Induced Depressive Disorder: When someone has a substance use disorder and a diagnosis of depression, it is called a co-occurring diagnosis or a dual diagnosis.
Co-occurring disorders are common, with up to 35% of adults in the United States who have a mental health disorder also having a substance use disorder.
In some cases, it can be challenging to determine which condition came first. Someone with a depressive disorder may turn to substances as a maladaptive coping strategy to feel better.
Or someone with a substance use disorder may first develop depression or other mental health disorders as a result of the psychological changes that can occur due to substance use.
Depressive Disorder Due to Another Medical Condition: Sometimes, people can develop depressive symptoms alongside another medical condition.
For example, it is common to develop depression after a traumatic brain injury (TBI).
Other conditions that can contribute to depression include, but aren’t limited to, Parkinson’s disease, brain tumors, multiple sclerosis, and endocrine disorders (e.g., hypo or hyperthyroidism).
Other Specified Depressive Disorder: This diagnosis is used when symptoms of depression are present, but don’t fit fully under one of the other depressive disorders, and the clinician communicates why the full criteria are not met.
For example, the depressive episode is not long enough to be classified under one of the other types.
Unspecified Depressive Disorder: This diagnosis is also used when symptoms of depression are present, but don’t fit fully under one of the other depressive disorders.
However, in the “unspecified” subtype, the clinician does not explain why the person did not meet criteria for any of the other types.
What Type of Depression Do I Have?
How Do I Know What Kind of Depression I Have?
A healthcare provider can help you understand which type of depression you have.
Many of the depressive and other mood disorders have signs and symptoms that overlap, which can make diagnosing challenging.
If you notice you or a loved one are experiencing signs and symptoms of depression, reach out to your healthcare provider for advice. Sometimes, general medicine providers like family practice or internal medicine providers can diagnose and treat depression.
However, if your symptoms are more complex, they may refer you to a psychiatric provider for a diagnosis and treatment.
What Are the Different Features of Types of Depression?
There are several different types of depressive disorders, as well as several other sub-types. For example, both perinatal depression and SAD are considered types of MDD.
With all forms of depression, it is important to note that it is more than one or two bad days. Those with a depressive disorder experience persistent symptoms for two or more weeks.
And some conditions, such as persistent depressive disorder and disruptive mood dysregulation disorder, require symptoms for one or two years, depending on the age of the individual.
What Is High-Functioning Depression?
*I moved this one over here because it was the only one not actually listed in the DSM-5
High-functioning depression refers to individuals who experience depression but are still able to maintain their day-to-day responsibilities. It is a term popularized by mainstream media and is not used in the DSM-5.
For example, individuals with high-functioning depression may outwardly appear to cope well and not display any obvious signs or symptoms of depression but struggle privately.
How Do I Get Diagnosed With Depression?
To get diagnosed with depression, the fastest path is to schedule an assessment with a behavioral health provider who can evaluate symptoms and recommend the right level of care. At Sandstone Care, admissions starts with a conversation and comprehensive clinical assessment to understand what’s been happening, how symptoms are affecting daily life, and what support is needed.
Because depression symptoms can overlap with anxiety, trauma, substance use, sleep issues, and other concerns, this kind of evaluation helps clarify what’s really going on so treatment matches the full picture.
You can also start with a primary care provider, who can screen for depression and refer you to psychiatry or therapy if symptoms are more complex.
Sandstone Care recognizes that depression is complex and offers several different evidence-based treatment options for mood disorders like depression. To explore options call (888) 850-1890.